Bringing Rare Procedures to Life: How the Clinical Environment and Simulation Work Together
By Diana Darr and Frank Ruggiero
In the realm of medical emergencies, certain procedures stand out for their rarity, urgency and inherent risks. Among these is the Blakemore procedure, a critical intervention utilized to stabilize esophageal hemorrhages.
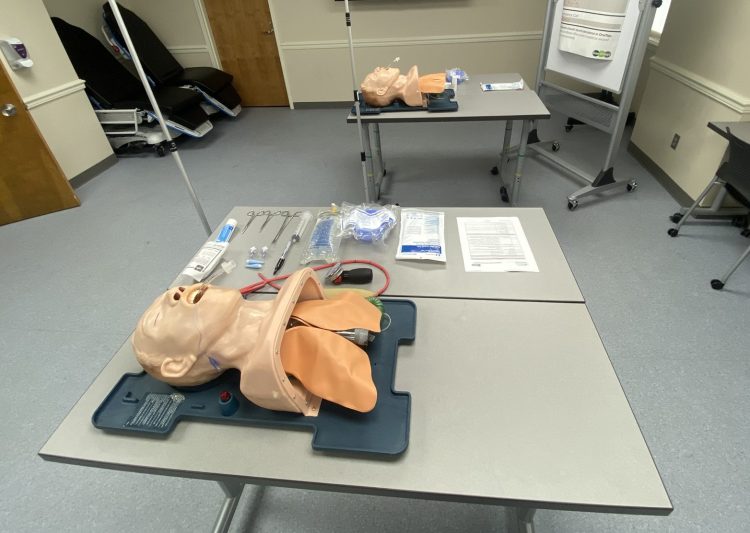
The Sengstaken-Blakemore Tube insertion, though infrequently performed, presents significant challenges due to its high-risk nature and the urgent need for intervention. These qualities position simulation as the perfect learning environment for mastering the complexities of the Blakemore tube procedure.
Enter UAB Clinical Simulation’s procedural simulation department. The Blakemore simulation came to be when a GI fellow reached out to simulation with a request for training on the procedure. The initial request was followed by other clinical teams’ involvement, including critical care and emergency medicine.
The simulation has since served as a unifying force for these distinct clinical areas, enabling them to train with the same simulation while making necessary modifications. Beyond replicating the procedure itself, the simulation fosters collaboration and knowledge-sharing across clinical domains.
The symbiotic relationship between the clinical environment and simulation has influenced practice across GI, critical care and emergency medicine.
For example, Chris Richardson, a critical care fellow, played a key role in this collaboration by facilitating the exchange of crucial information and tools between clinical practice and simulation.
Additionally, Andrew Bloom, assistant professor and director of the Emergency Simulation Fellowship in the Heersink School of Medicine’s (HSOM) Department of Emergency Medicine, runs simulations for emergency medicine students, residents, faculty members and departments, while also conducting simulation education research within the emergency department (ED).
“Over the last few years, we have focused on developing a full range of clinical cases for our emergency medicine residents in immersive sim,” Bloom said, noting that this also involves case writing that inter-professionally incorporates nursing students and pharmacy residents. “We have also looked to develop a procedural simulation curriculum. We run resident simulations monthly, and in the last two years, Lisa (Bergman, UAB Clinical Simulation’s director of procedural simulation) and I have tried to expand the procedures available to our residents and create a longitudinal curriculum. The procedural simulations have been developed to address a need for our ED residents to be ready for anything, have procedural competency and have the ability to practice in a simulated and safe environment.”
Bloom said the residents’ feedback has been amazing—and even serendipitous, as it was this very feedback that inspired the creation of the Blakemore simulation.
“Interestingly enough, Lisa was already in talks with the MICU (medical intensive care unit) to develop the task trainer, and I expressed our interest in our ED residents getting training,” Bloom said. “We did it for the first time last year in our procedural simulation curriculum with great feedback, and we were excited to add it to our rotation of procedures. After our sim, we had a massive GI bleed in our ED, and our residents and faculty who helped facilitate were present. They noted that the procedural simulation allowed them to be prepared and act.”
Jordan Newman, assistant professor of pediatrics and assistant program director of HSOM’s Pediatric Critical Care Fellowship Program, applied his procedural simulation experience to facilitate a Blakemore simulation at Children’s of Alabama, utilizing UAB Clinical Simulation’s equipment loan process.
“By witnessing a thorough and well-crafted simulation through Clinical Simulation and having the opportunity to borrow their equipment, I was empowered to craft a tailored simulation experience for the Pediatric Critical Care Fellows in the Pediatric Simulation Center at Children’s,” Newman said. “The Blakemore tube training session and equipment we were able to utilize helped foster an innovative learning environment that I believe will help advance the care of pediatric patients.”
According to Bergman, this collaboration exemplifies UAB Clinical Simulation’s dedication to elevating patient safety.
“The Blakemore procedure simulation serves as a testament to the department’s collective efforts to standardize processes and enhance the quality of patient care,” she said. “Together, we are shaping the future of health care, one simulation at a time.”
UAB Medicine’s Clinical Simulation program offers opportunities for individuals and teams across UAB Medicine and beyond to practice before they deliver care. We encourage all who provide and support patient care to “SimFirst.” Together, we can put our patients’ safety first.




0 Comments