‘Don’t call them dummies’: Manikins bring realism to simulation
Put simply, manikins are model patients.
They’re also some of UAB Clinical Simulation’s most powerful and sophisticated learning tools.
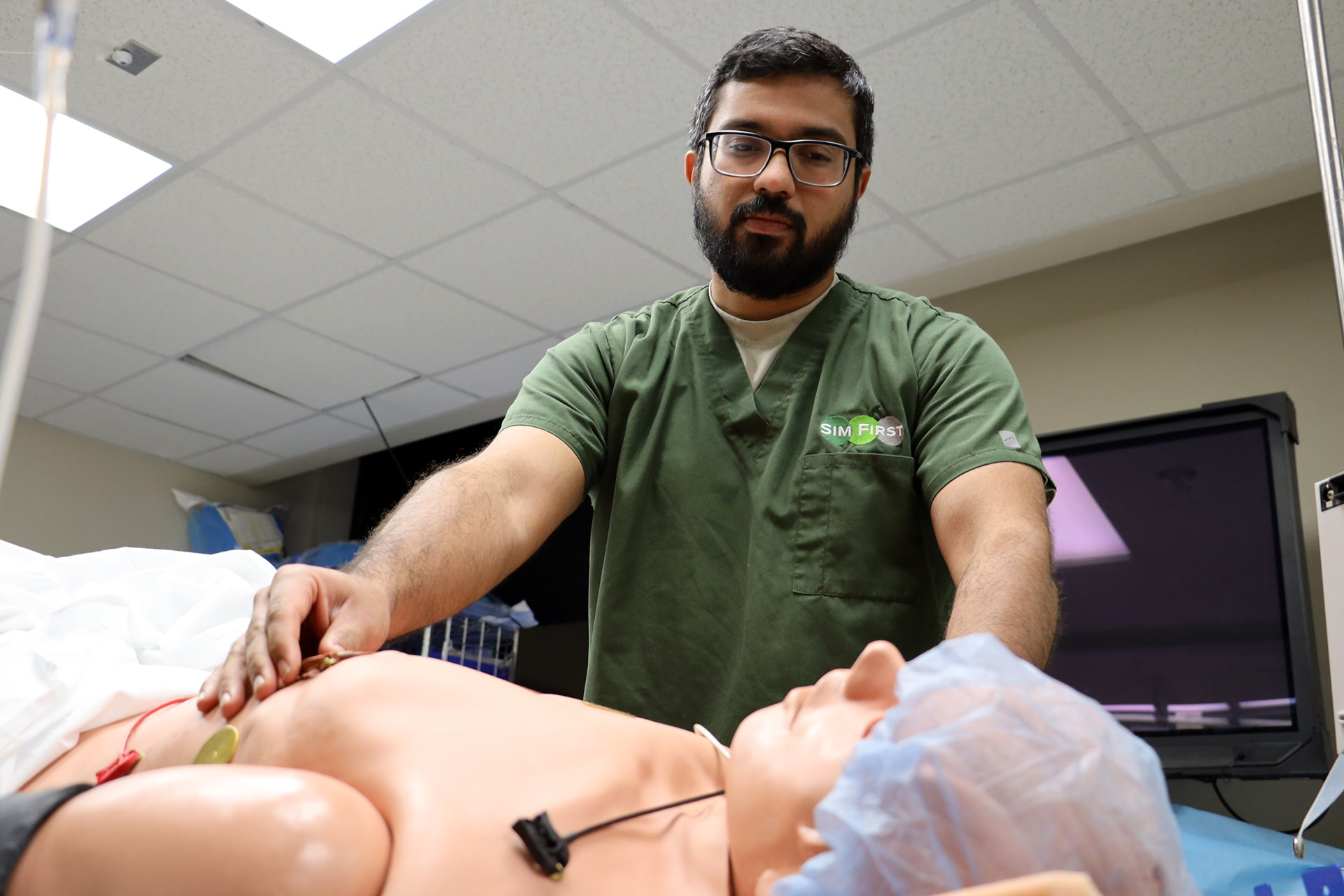
As patient simulators, manikins mimic human anatomy and physiology, allowing learners to practice clinical skills in a psychologically safe environment, thus improving patient safety. In that regard, preparation is key — not just for learners, but the manikins themselves.
When an immersive simulation is being developed, it’s up to UAB Clinical Simulation’s operations team to ensure the manikins are up to the task.
“Not only do we maintain the manikins and make sure they’re clean and operating properly, but we also prepare them in all sorts of ways to bring realism to the simulated scenario,” said Ben Whitaker, manager of Clinical Simulation operations.
For each simulation, Whitaker and his team dive into the scenario background.
“We explore everything we need to know — who the patient is, what they’re experiencing, whether they’re arriving in the emergency department or if they’re in a clinic or even outside, whatever the case might be,” Whitaker explained.
This informs such details as the assigned manikin’s gender, whether it requires moulage (e.g., special effects make-up to simulate injuries and illnesses) and how it is dressed.
“Say the scenario depicts a car accident,” Whitaker said, “If the driver’s side is impacted, we’ll apply moulage and makeup to the left side of the manikin,” Whitaker said. “We can simulate bruising, lacerations, bone fractures and an assortment of bodily fluids; it’s a very interesting job, to be honest.”
If the scenario takes place in a hospital setting, the manikin will be dressed accordingly in a patient gown. Emergency department simulations see manikins garbed in street clothes. If the sim starts with the patient under anesthesia, Whitaker and his team will intubate the manikin and ensure it’s connected to all the appropriate equipment. If the scenario begins with the patient hooked up to a monitor, operations will attach the appropriate EKG leads. Other times, learners may find defibrillator pads already attached.
“There are all sorts of things we can do to bring realism to the scenario,” Whitaker said.
That includes the control room.
From there, the operations team controls the manikin itself, including such key aspects as vital signs, breathing and pulse, along with others that learners might not even anticipate, like sound effects, vocalization and blinking.
“A lot of times, the patient is talking to or interacting with the health-care providers in the room, so setting up the patient’s voice is a whole other component,” Whitaker said, noting that voice modulators are often used to disguise the operator’s voice.
In that regard, a scenario’s level of realism is literally the sum of its parts. Oftentimes, first-time learners are surprised by the manikins’ lifelike capabilities.
“Most of the time, if someone’s never seen a patient simulator, they come in and call it a dummy, and I say, ‘Well, that hurts their feelings. They’re patient simulators,’” Whitaker said. “But usually, when I explain what they’re capable of, that changes their perspective a bit. It’s cool to see their reaction or after putting their fingers on the pulse and feeling how realistic it is or being able to grab a stethoscope and actually hear a heartbeat or breathing. And the first time they see a manikin blink? They’re usually pretty blown away by that.”
Want to put Clinical Simulation’s patient simulators to use? Find out how here.



0 Comments